The need for pharma to deliver better value for money through medication has perhaps never been more pressing. Healthcare costs are rising twice as fast as GDP growth in many countries and, in the US, nearly half of the adult population has at least one chronic illness (1).
Against this background, it is estimated that half of medications for chronic diseases are not taken as directed (2), and many struggle to continue with their treatment as prescribed.
Evidence indicates that providing targeted support for those chronic patients on treatment can positively impact adherence and outcomes, in turn generating value for health systems through fewer hospitalisations and lower morbidity and mortality rates. The benefit from greater adherence appears to be a win-win, yet in our experience, only a minority of pharma companies are effectively realising the opportunity for patient support. Research shows that only a small proportion of potentially eligible patients are currently using support programmes, primarily due to a lack of awareness regarding their availability. (3)
This article is written by Wavestone’s patient experience experts, exploring how pharma companies can do more for people that are on their treatment, and what practical steps can be taken to get there.
What is the case for patient support delivered by pharma?
The case for actively providing these services revolves around 3 main ideas:
Patient beliefs, attitudes, and preferences regarding healthcare, treatment options, and lifestyle choices play a significant role in treatment adherence and engagement, which in turn impact on outcomes.
“It is critical to see the person behind the patient. This is the only way to truly understand the complex mix of physical, emotional and social challenges someone living with a chronic condition encounters on a daily basis. These challenges can significantly impact quality of life and ability to adhere to, and persist with, the treatments prescribed to them”. Dr Nicola Davies, Behavioural Scientist and patient support expert.
These challenges vary at an individual level and are often further impacted by societal factors that differ across borders. Factors such as health literacy, support networks including family centricity and social stigma of some diseases, play a greater role in some countries than in others.
Organised Patient Support Programmes (PSPs) provide the means for pharma companies to address individual needs in a coordinated way, with the more sophisticated organisations timing the support according to the individual, with delivery at the precise moment they need it.
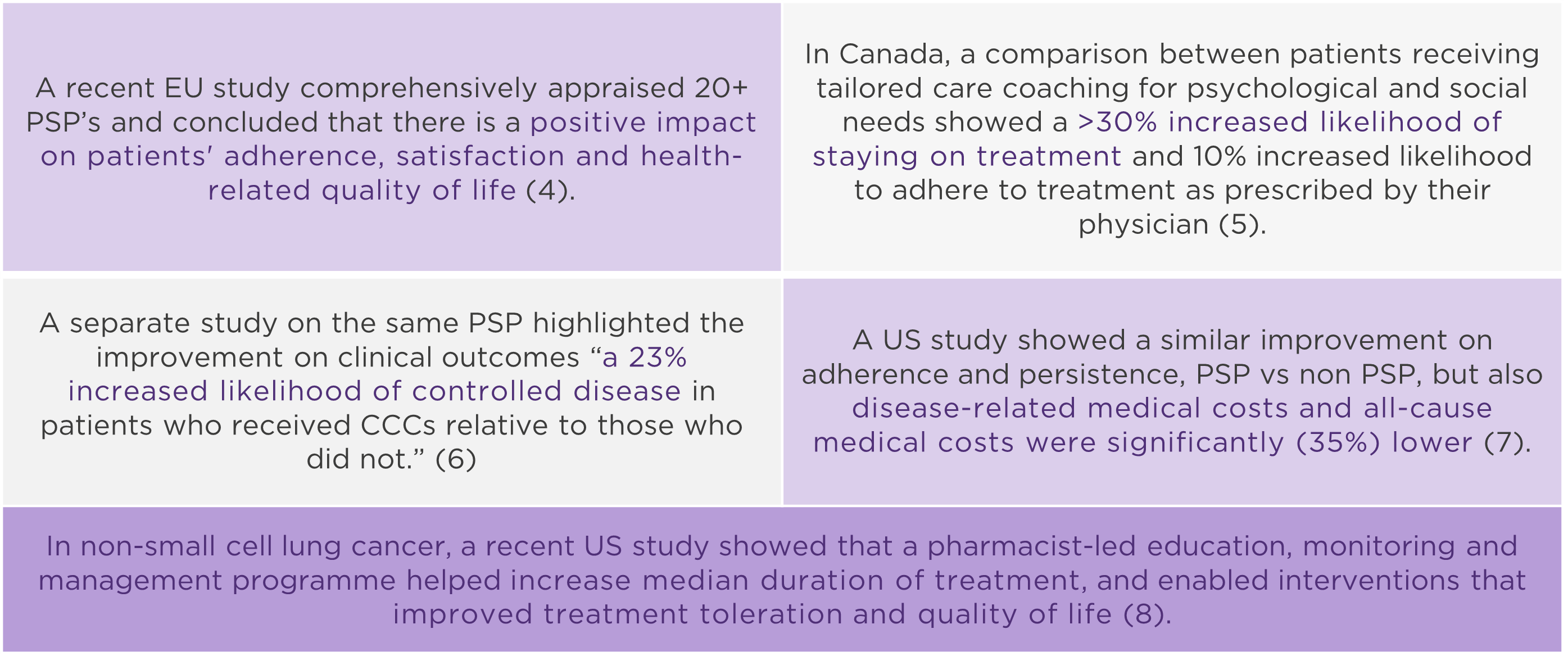
There is growing evidence that PSPs can have a positive impact on patient experience and clinical outcomes. Here are five examples:
Pharma has the advantage over other players (new tech companies, health care providers, patient organisations) of truly understanding their medications and treatment journeys.
As such, they are arguably best placed to design programmes of support that complement – not impinge upon – health provision and positively impact on outcomes. And, unlike national governments, big pharma has the advantage of being able to deliver patient-focused services internationally.
There is additional value to be gained beyond better patient outcomes: deeper patient insights, real world evidence, improved patient centricity, reputation and ultimately improved bottom line through greater treatment persistence.
“Traditionally, holistic patient support is often not seen as the ‘space’ for pharma companies, but they are in the unique position of having the expertise, capability and incentive to deliver impactful improvements – many are already doing it.” Magnus Franzen, patient outcomes & experiences expert.
Delivering patient support effectively – 6 practical recommendations
Despite the investment, there are many examples of patient support solutions that fall short of making a difference and often centre around single solutions such as apps or educational websites.
By contrast, we have seen that integrated programmes based on need really can positively impact on patients. Drawing on our experience across multiple big pharma, we make six recommendations to avoid common pitfalls and effectively deliver patient support:
Let us know if you have a different perspective on this, and how pharma could do more for patients:
Glen McCracken: Patient services specialist
Magnus Franzen-Rossi: Patient outcomes & experiences expert
Sharon Yau: Patient solutions design & execution expert
- Raghupathi (2018). An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5876976/
- Fernando-Lazaro et al (2019). Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study | BMC Primary Care | Full Text (biomedcentral.com);
- Fierce Pharma (2021). Pharmas’ return on $5B spent yearly on patient support programs? https://www.fiercepharma.com/marketing/pharmas-return-5-billion-spent-yearly-patient-support-programs-only-3-use-survey
- Sacristán et al (2022). The Impact of Patient Support Programs in Europe: A Systematic Literature Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9584873/
- Marshall et al (2018). Impact of the Adalimumab Patient Support Program’s Care Coach Calls on Persistence and Adherence in Canada: An Observational Retrospective Cohort Study https://pubmed.ncbi.nlm.nih.gov/29519714/
- Bessette et al (2018) Impact of the Adalimumab Patient Support Program on Clinical Outcomes in Ankylosing Spondylitis: Results from the COMPANION Study Impact of the Adalimumab Patient Support Program on Clinical Outcomes in Ankylosing Spondylitis: Results from the COMPANION Study | Rheumatology and Therapy (springer.com)
- Brixner et al (2019). Patient Support Program Increased Medication Adherence with Lower Total Health Care Costs Despite Increased Drug Spending Patient Support Program Increased Medication Adherence with Lower Total Health Care Costs Despite Increased Drug Spending | Journal of Managed Care & Specialty Pharmacy (jmcp.org)
- Khrystolubova et al (2020). Pharmacist-led patient education and adverse event management in patients with non-small cell lung cancer receiving afatinib in a community-based, real-world clinical setting: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6886115/pdf/10.1177_1078155219833441.pdf
- M. Franzen-Rossi. From adherence to outcomes: The Patient Support Programme of the future: https://wwa.wavestone.com/en/insight/from-adherence-to-outcomes-the-patient-support-programme-of-the-future/